Application in a Traumatic Orbital Wound

Anthony N. Dardano, DO
Chief, Plastic Surgery Trauma – Delray Medical Center – Ft. Lauderdale, FL

Pre-operative assessment

Last follow-up (Week 7)
Results
- Rapid reperfusion of tissue surrounding graft placement
- Wound closure achieved
- Near 100% epithelization
Patient details
66-year old male
Medical history
PMH significant for glaucoma of left eye
Case details
- Right orbital trauma s/p motor vehicle accident
- Exposed right frontal bone
- Complete loss-of-vision right eye
- Obtunded; GSC 14
- Multiple nasolabial lacerations
- Anterior forehead laceration
- Nondisplaced nasal fracture
- Frontal bone fracture
- Right frontal branch of facial nerve non-functional
- Complex avulsion laceration of right forehead extending distally and laterally to right zygomatic and maxillary regions
Application photos

Initial Presentation (Day 0)
- Complex avulsion laceration of right forehead extending distally and laterally to right zygomatic and maxillary regions

Initial Debridement (Day 0)
- Procedure: Wound debrided to remove necrotic tissue and lavaged to remove foreign material
- Defect size: 12 cm x 3 cm x 2 cm
Peri-operative Imaging (Day 0)
- Perioperative angiography (ICG SPYTM) revealed necrotic tissue with minimal perfusion to the facial flaps

Myriad Matrix Placement (Day 0)
- A 7 x 10 cm 2-layer Myriad Matrix was trimmed to size and secured to the wound bed
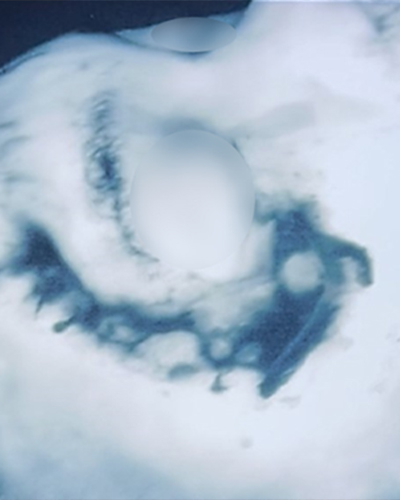
Repeat ICG-SPYTM Angiography (Day 2 from Index Surgery)
- Return to OR
- Second round of debridement performed
- Intra-op ICG SPY™ imaging system angiography revealed rapid reperfusion to tissue surrounding the graft placement

Final closure (Day 2 from Index Surgery)
- An additional Myriad Matrix graft secured to wound bed
- Fasciocutaneous flap from zygomatic arch elevated and mobilized to allow for tissue closure
- Final closure performed
- Small distal opening to allow for drainage

Follow-up (Day 3 from Index Surgery)
- Wound closure appears intact
- No signs of necrosis
- Xeroform™ in place for drainage

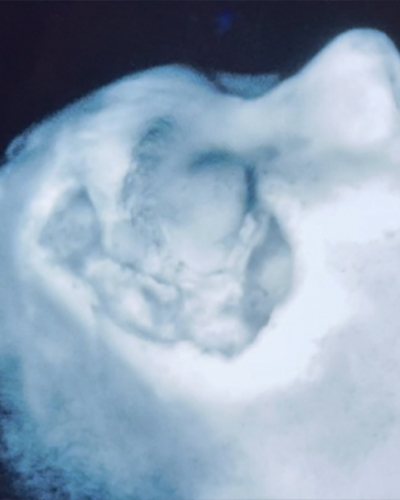
Follow-up (Week 7)
- Wound closure achieved
- Near 100% epithelization
Results may vary.
Dr. Dardano has a consultancy agreement with Aroa Biosurgery Limited.
Xeroform™ and ICG-SPY™ are trademarks and property of the respective owners.